 Video Courses
Video Courses Video Courses
Video Courses
Abbreviations: PCI percutaneous coronary intervention, hs-cTn high sensitivity cardiac troponin, STEMI ST elevation myocardial infarction, ED emergency department, ER emergency room
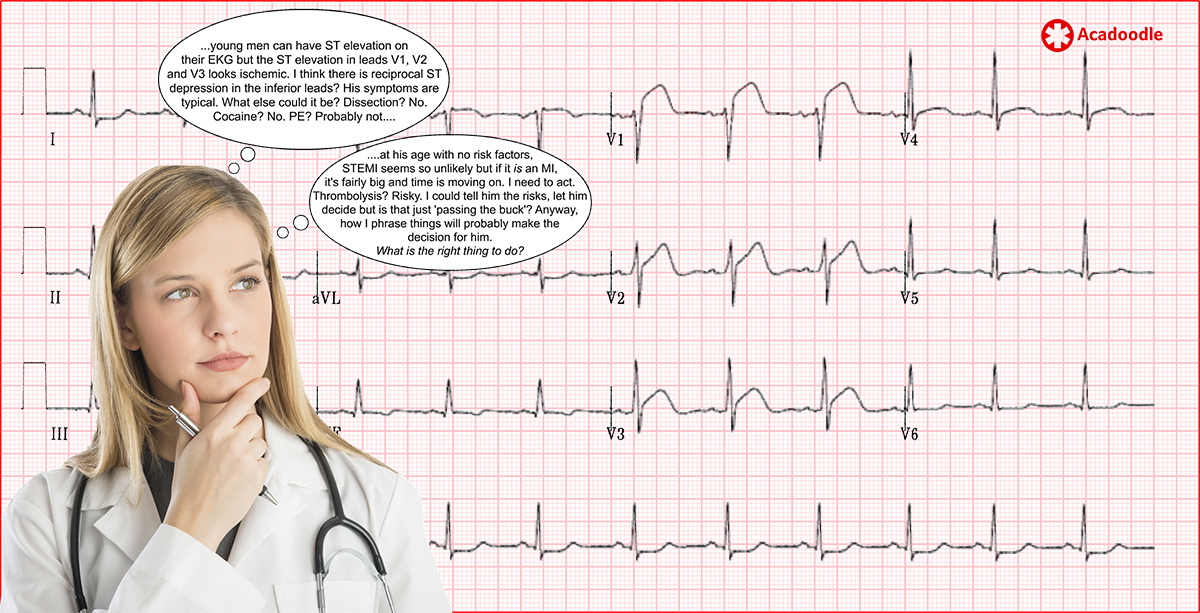
In the dead of night, during a violent storm, a 22 year old tourist is brought by friends to the ED(ER) of a remote small acute general hospital. He is visibly distressed and complains of a three hour history of central chest pain which is ongoing at presentation. There is no history of trauma. The admitting registrar, an excellent junior doctor, feels that the patient's chest pain is typical of cardiac ischemia. The patient’s ECG at presentation is shown below.

There is no facility for percutaneous coronary intervention (PCI) at the hospital. There is no 'out of hours' cardiology consult service on site. With the storm, there is no prospect of getting the patient to a PCI-capable hospital within the two hours following 'first medical contact' (FMC)*. His SpO2 on room air is 98%. Blood pressure is normal and equal in both arms. Consumption of drugs of abuse is denied. Urine toxicology is positive for THC but negative for cocaine metabolites. While under review, the patient experiences a short run of non-sustained ventricular tachycardia on the monitor. Because of concerns over ‘door to needle time’ the junior doctor feels under pressure to act, trusted experienced voices around her in the resuscitation room, however, urge caution.
* In the case of a patient presenting to a non-PCI-capable hospital with an STEMI, if transfer to a PCI-capable hospital cannot be achieved within two hours of FMC, in the absence of contraindications, intravenous thrombolytic therapy is indicated (1).
The doctor takes a moment to think.
The high sensitivity cardiac troponin (hs-cTn) result is then called through to the resuscitation room. The plasma troponin level is grossly elevated, twenty fold above the cut-off level for the assay in use in her hospital. Portable CXR is clear and d-dimer is negative. The pressure to act mounts.
Preparations are made for administration of an intravenous thrombolytic agent. The risk of hemorrhagic stroke is explained to the patient and consent is obtained.
The Junior doctor hesitates. 'Wait. This isn't right. I need to call the boss'. The registrar phones her senior, an experienced general physician. The senior asks the registrar to send her an image of the ECG by phone. She quickly reviews the ECG, agrees that it looks like an acute STEMI, confirms that antiplatelet agents have been given but tells the junior doctor not to administer the thrombolytic and that she will be with her shortly.
Like her junior, the senior doctor will be aware that there are 'mimics' of STEMI. However, she will also be aware that there may be a possible explanation for this clinical scenario unknown to her. We have all been caught out by an 'unknown unknown'. Even if she cannot establish the underlying cause of this presentation with any degree of certainty, influenced by the level of doubt present, she will ask herself, if this is an STEMI what is the actual benefit of administering a thromboyltic in this circumstance, what will it cost the patient if I don't administer it? Is the risk/benefit profile known in this age group? She will seek advice from a specialist center while ultimately taking responsibility for any decision made.
The fictitious scenario described here could end in a number of ways. The case presented is based on a very similar ‘real-life’ case I encountered some years ago. The ECG shown above is modelled on my memory of that young person’s ECG at presentation, with ST changes in the septal leads highly suggestive of AMI (see video below). The history is identical and there was a grossly elevated cardiac troponin concentration at presentation. The final diagnosis was focal (septal) myocarditis. The doctors managing the case were not aware of the existence this condition. In focal myocarditis, ECG changes, confined to the region of the heart affected, can result in ST changes in a single vascular territory mimicking acute STEMI. In the timeframe involved, the doctors felt that they had to act and a thrombolytic agent was administered intravenously. Following transfer to a specialist center, angiography demonstrated normal coronary arteries. Cardiac MRI was consistent with the presence of focal septal myocarditis and this diagnosis was confirmed on endomyocardial biopsy. The patient survived, with no adverse consequences resulting from the thrombolysis. After the event, the patient’s plasma troponin level returned to the normal range. Subsequently, it was determined that the patient had had a history of probable viral gastroenteritis three weeks prior to the initial presentation to the ER. Focal myocarditis is believed to be triggered by a variety of viral infections and may follow viral gastroenteritis. In my experience, when the 'dust has settled' in difficult cases such as this, a retrospective history focused by the final diagnosis will often reveal something 'highly significant' initially 'missed'. Hindsight will always have perfect 20:20 vision. Even if the history of possible viral gastroenteritis had been available in the resuscitation room, I doubt if it would have altered the decisions made.
The patient described here had experienced an 'acute myocardial injury' as evidenced by the rise and fall in high sensitivity troponin level. However, the injury was secondary to focal viral myocarditis and not type I myocardial infarction.
As a teaching point, the registrar felt that the ST changes in the septal leads where consistent with STEMI . What is she seeing when looking at these leads?
All linked papers are free access. We want you to read them. We would welcome suggestions of links to informative free access case reports/review papers/updates from interested learners.
Munguti et al. ST Segment Elevation is not always Myocardial Infarction: A case of focal Myopericarditis. Case Reports in Cardiology. 2017 https://www.hindawi.com/journals/cric/2017/3031792/
- An excellent 'real-world' case description, ECG at presentation is indistinguishable from that of an inferior type I myocardial infarction.
Nozari Y et al. Focal Myocarditis as a Rare but important Differential Diagnosis of Myocardial Infarction; a Case Series. Emergency 2016;4(3):159-62. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4902212/
- An informative case series, note the dynamic change in hs-cTn concentrations.
Testani JM et al. Focal Myocarditis Mimicking Acute ST-Elevation Myocardial Infarction: Diagnosis Using Cardiac Magnetic Resonance Imaging. Texas Heart Inst J 2006;33(2):256-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1524714/
- Dramatic dynamic regional (anterior) ST elevation on the ECG. MRI images of focal myocarditis.
Cooper LT. Myocarditis. N Engl J Med. 2009;360(15):1526-38. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5814110/
- An informative general review of myocarditis
Brownfield J and Herbert M. EKG Criteria for Fibrinolysis: What's Up with J Point? West J Emerg Med 2008 9(1): 40-2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2672223/
(1) Our comment on 'First medical contact' and thrombolysis in non-PCI-Hospitals
O'Gara PT et al. 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction. Circulation 2013;127:e362-e425. https://www.ahajournals.org/doi/full/10.1161/cir.0b013e3182742cf6
DisclaimerPrivacy PolicyTerms of UseData Deletion© Acadoodle 2026