 Video Courses
Video Courses Video Courses
Video CoursesThis article was originally published online in November 2018 in the aftermath of the H1N1 pandemic and as we approached the one hundredth anniversary of the end of the First World War. Today, in Dublin, as in many other cities across the world, we are in partial ‘lockdown’ in an attempt to minimise the impact of the COVID-19 pandemic. Fortunately, it appears at this time that ARDS is not occurring in the young or in pregnant women at as high a frequency as was observed during the H1N1 pandemic. In fact, the manifestations of COVID-19-induced ARDS, reported by our Chinese colleagues, seem to be somewhat different to those seen in H1N1 infection. (Article here)

The Last General Absolution of the Munsters at Rue du Bois (Fortunino Matania)
It was known in Sir William Osler's time that severe inflammation in the lung from any cause may give rise to a clinical syndrome characterised by generalised pulmonary edema. In a high proportion of cases, irrespective of the initiating factor, the clinical course proved relentless with progression to respiratory failure and death. This syndrome gained infamy during the Great War.
The first major deployment of chemical weapons on the battlefield occurred on the Eastern and Western fronts during World War I. Inhalation of irritant poison gas resulted in the deaths of many soldiers from respiratory failure, a condition referred to at the time as 'shock lung'. The physical and psychological suffering of the soldiers was immortalised by Wilfred Owens description of a gas attack on the Western front.

Phosgene gas deployed at Fromelle near the Somme was believed to be responsible for many Australian and British deaths (centre image, 1916). Pictured right: 2nd Lt Wilfred Owen M.C.
The initial agent deployed, chlorine gas, was highly irritant and exposure induced violent bouts of coughing limiting the dose inhaled by soldiers. Phosgene gas was developed as an alternative. Phosgene was less irritant, thereby ensuring soldiers were unaware of the exposure and inhaled a larger dose before using their masks. The inhaled agent induced an inflammatory response in the lung and, often after a latent symptom-free period of two to three days, was followed by death from intractable pulmonary oedema.

Men of the 101st airborne call in helicopters to evacuate their wounded comrades. Medical evacuation from the battlefield reached its zenith in the Vietnam war with unexpected consequences.
The first major incursion into Vietnam by the US marines took place in the coastal region of Da Nang and, after a time, resulted in heavy casualties, wounded and dead. Following on from the lessons of the Korean war, the US military were determined that when soldiers were wounded on the battlefield they would be evacuated as quickly as possible to receive immediate medical attention, including fluid resuscitation for blood loss. To their astonishment, this approach seemed to worsen outcome. Many young men died in the days and weeks post evacuation from intractable pulmonary edema and respiratory failure. In many cases, the initial wounds did not involve the lungs but distant parts of the body. The pulmonary condition killing these men ('Da Nang lung') was so similar to the delayed 'shock lung' of phosgene gas attacks in World War I, that for some time the military were convinced that the Viet Cong were using a phosgene gas-like agent in the conflict. In reality, generalised pulmonary edema was occurring secondary to injuries distant from but linked to the lungs by a mechanism unknown. The tendency to develop pulmonary edema may have been aggravated by aggressive fluid replacement.
The recent H1N1 influenza pandemic emphasised how little progress has been made in the understanding and management of ARDS. Those of us involved in managing patients during the outbreak had a similar experience to the military doctors in the two wars discussed above. Avian influenza is associated with a relatively high rate of development of ARDS in pregnant women. The striking feature of this complication in case series reported was the variability in the progression of the condition in these women. The clinical course varied from complete resolution to progressive lung destruction and death. We still understand very little concerning the link between inflammation and ARDS and we have no idea why the link is so pronounced in pregnancy.
It seems that in susceptible individuals, acute severe inflammation of the lung (direct ARDS), or inflammation in organs distant from the lung (indirect ARDS), can result in generalised increased permeability of the alveolar capillary membrane to fluids. To understand ARDS perhaps we need to ask a question. Under normal circumstances, how are the air filled alveoli kept free of fluid in lungs which are themselves full of fluid?
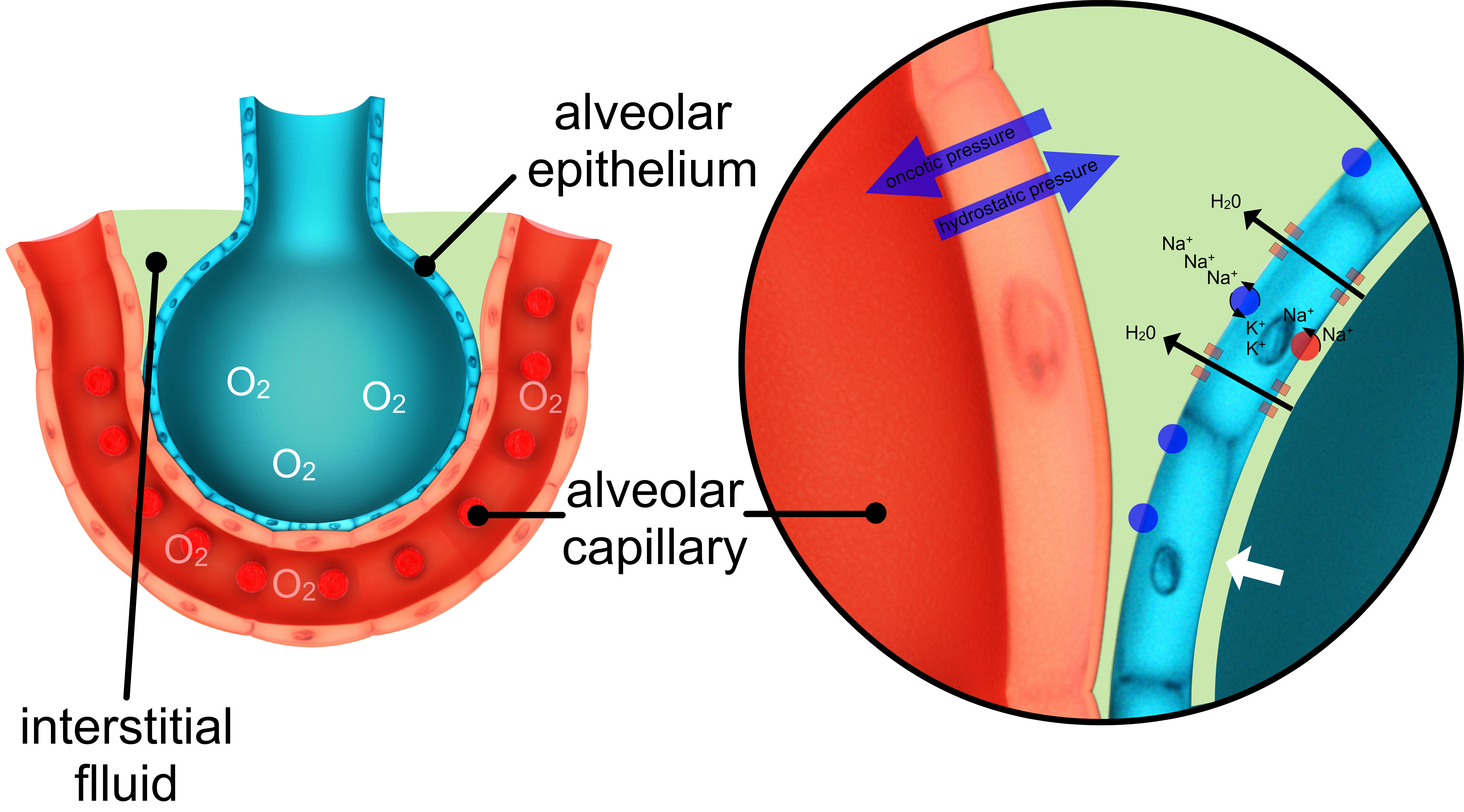
(Image above) The formation of interstitial fluid in the lung from pulmonary capillaries is determined by the balance between Starlings forces (blue arrows) acting on the fluid in the capillaries. Under normal circumstances, the movement of fluid between the interstitial compartment and the alveoli is tightly regulated. Sodium ions enter the alveolar epithelial cells from fluid in the alveoli facilitated by sodium channels present in the apical membrane of the cells. Energy dependent Na+/K+ pumps (blue spheres) generate an osmotic gradient by extruding sodium ions from the cytosol of the alveolar epithelial cells into the interstitium. Possibly facilitated by aquaporins, water moves along the osmotic gradient generated by this process (black arrows). This results in the maintenance of a very thin layer of fluid (white arrow) on the alveolar luminal side of the alveolar epithelium.
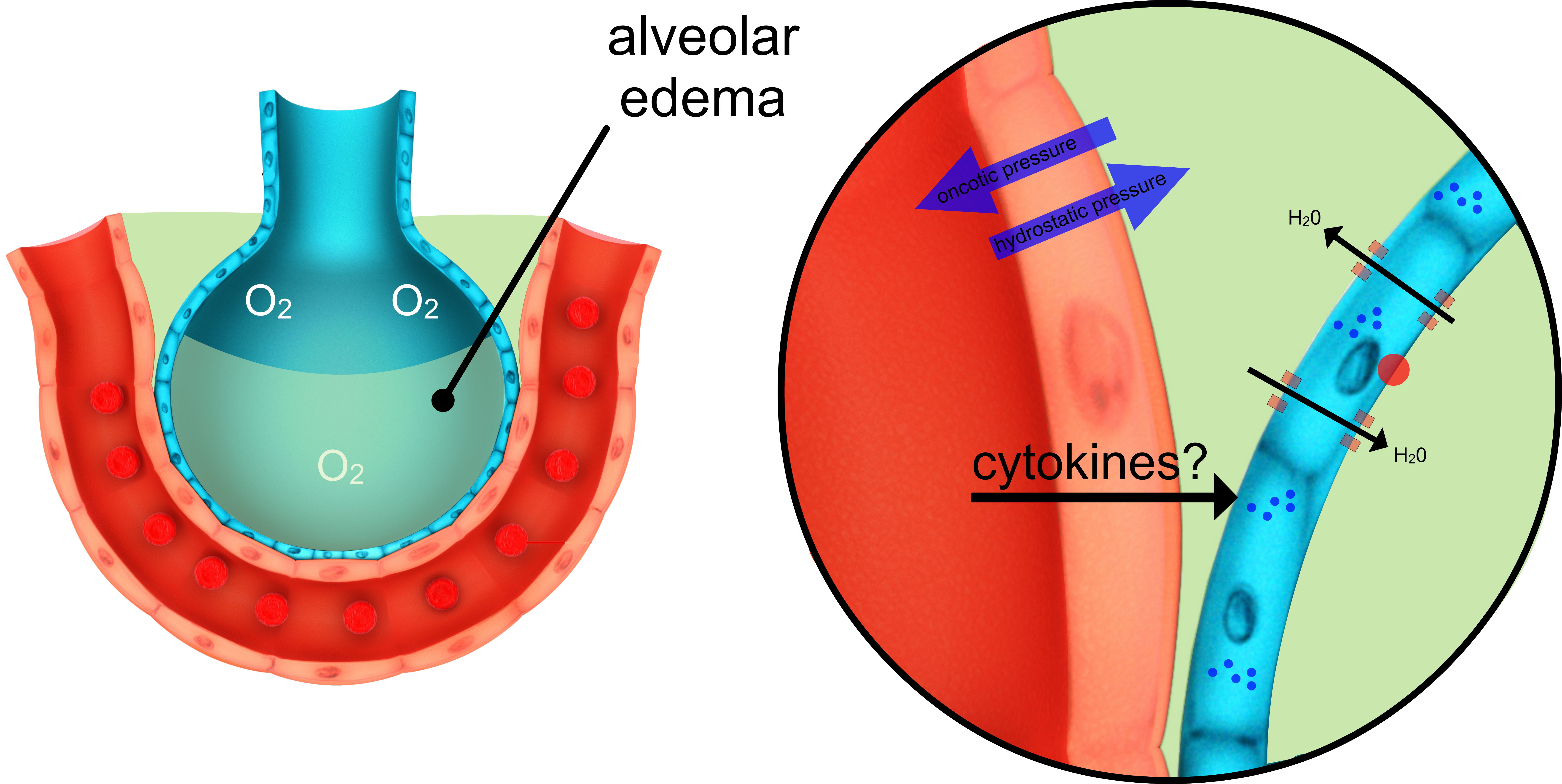
(Image above) Recent evidence suggests that cytokines released from macrophage in response to viral pneumonitis can inhibit the assembly and insertion of the energy-dependent Na+/K+ pump into the alveolar cell membrane (Peteranderl et al, JCI 2016, 126(4) p1566). Loss of the osmotic gradient discussed above would be expected to lead to fluid accumulation in the alveoli. There is experimental evidence that phosgene gas increases alveolar capillary permeability by a similar mechanism.
Intuitively, one would assume that direct destruction of alveolar epithelium with loss of all semblance of a permeability barrier must play a role in cases of direct ARDS. For example, weaponised chlorine gas reacted with water in the tissues to form hydrochloric acid and presumably destroyed elements of the barrier instantly. However, the cytokine hypothesis as outlined above is attractive. It would offer a mechanism by which distant severe trauma/inflammation (distant from the lungs) can be linked to the development of indirect ARDS.

Like civilisation, ARDS is difficult to define but most of us know it when we see it.
Recently, the diagnostic definition of ARDS has changed. The 'Berlin' definition (a European initiative endorsed by the American Thoracic Society), captures the main features of this historic syndrome.
The presence of ARDS is defined by new or worsening respiratory symptoms 1) within seven days of a recognised clinical trigger* with 2) bilateral opacities on chest X ray not fully explained by effusions, lobar lung collapse or nodules and 3) the respiratory distress cannot be fully explained by cardiac failure or fluid overload (in the best estimation of the attending physician).
Ventilatory requirements retain a role in the new definition. To diagnose ARDS we must show that a certain level of PEEP (positive end expiratory pressure) is required to generate adequate arterial oxygenation. The degree of difficulty in oxygenating the patient is used as a measure of the severity of the condition.
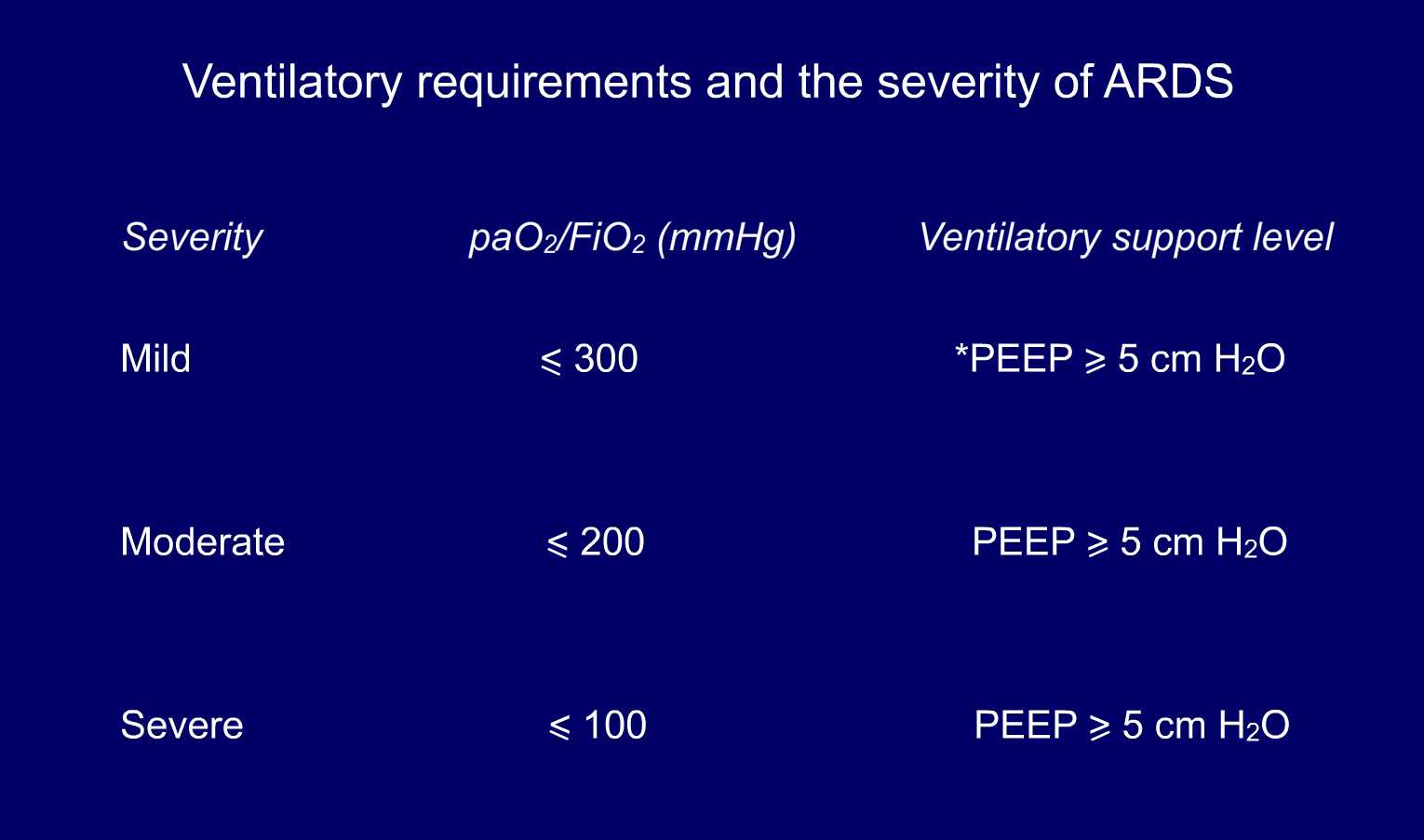
(mmHg = 7.5 x kPa).*PEEP (positive end expiratory pressure) or CPAP (continuous positive airway pressure) in mild cases.
Exclusion of heart failure as a cause of respiratory distress remains a central part of the diagnosis of ARDS. In the older definition this required placement of a Swann Ganz catheter with direct measurement of pulmonary capillary wedge pressure. This is no longer required. Clinical judgement, usually complimented by echocardiography, is considered sufficient. Also, the term acute lung injury (ALI) is now defunct. The new definition of ARDS retains a central role for the chest X ray in diagnosis.
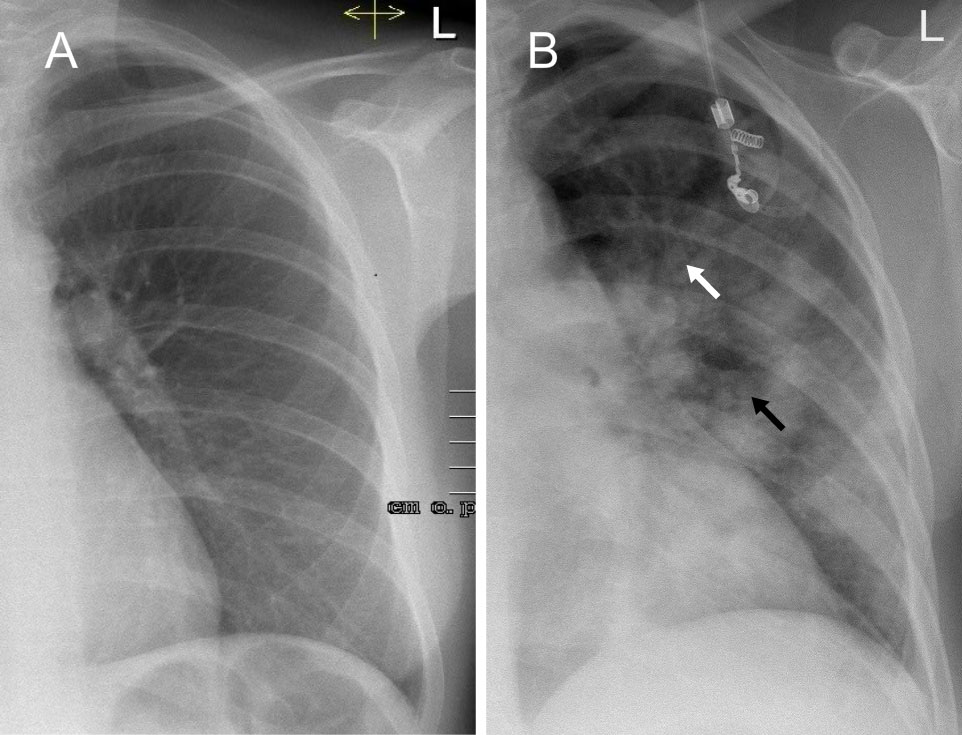
Compare a normal CXR (A) to the 'froth corrupted lung' of ARDS (B). In (B) a pattern of shadowing consistent with alveolar consolidation is seen. Multiple 'fluffy' areas of shadowing with soft edges are present. The process appears to fan out from the hilum. Air bronchograms (white arrow) can be seen indicating that the airways are spared (filled with air rather than fluid). There may be evidence of acinar shadowing (black arrow). One cause of such an alveolar pattern of consolidation is alveolar edema.
*Some recognised triggers of ARDS
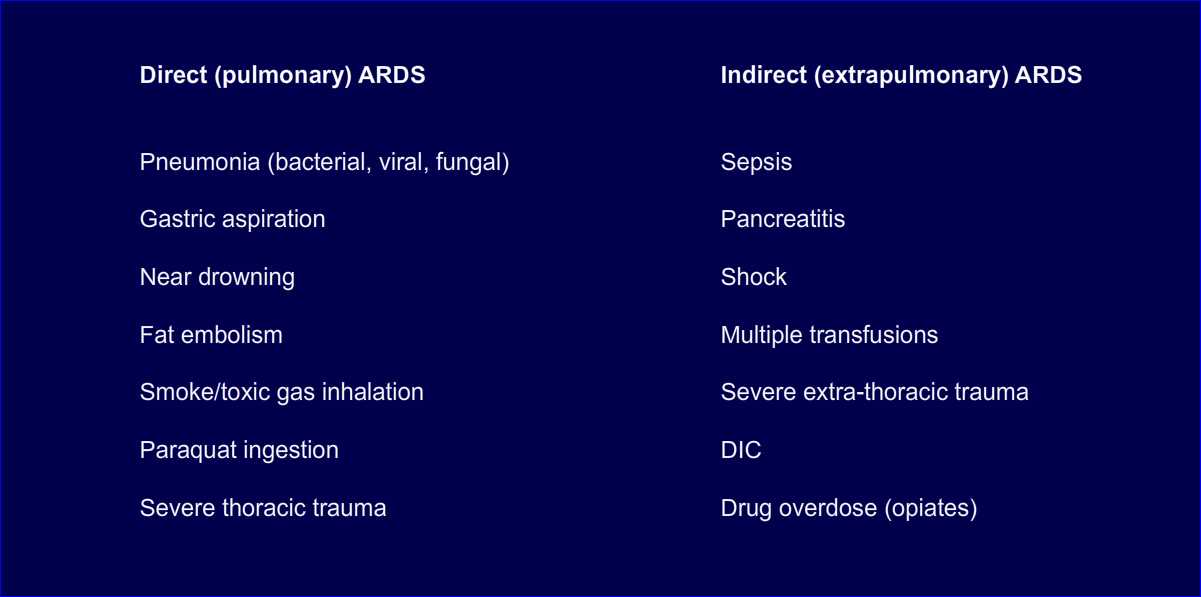
DIC: disseminated intravascular coagulation
There is no specific treatment for ARDS. As a key feature of the syndrome is fluid accumulation in the alveoli, intensivists tend to 'run the patient dry' using inotropic support as necessary. When possible we treat the presumed underlying trigger of the condition aggressively (for example antivirals in cases of influenza). Careful attention is paid to the technique of ventilatory support employed in the acute phase as there is some evidence that excessive airway pressures generated during mechanical ventilation may worsen the long term outcome. Perhaps surprisingly, anti-inflammatory agents, including steroids, are of no benefit. Recovery is unpredictable and, after supportive measures have been instigated, is largely in the lap of the gods. A high proportion of patients will die either of respiratory failure in the acute phase or progress to intractable pulmonary fibrosis with increasing loss of lung compliance rendering mechanical ventilation difficult. In those who survive, the condition may resolve completely or evolve into a debilitating chronic restrictive lung disease characterised by pulmonary fibrosis.
Dr John Seery 06.11.2018, updated 07.04.20
This piece is dedicated to the memory my great-grandfather John ‘Jack’ Kelly, a veteran of the Great War and his three brothers killed in action in that conflict, Edward (Armentiéres, 1914), James (the Somme, 1916), Michael (Chambrai, 1917) and Jack’s brothers-in-law, Michael and James Gorman. Michael was killed in action at Suvla Bay in 1915. James suffered life-altering injuries inflicted during the gas attacks at Passchendael. All from Kiladreenan, Newtownmountkennedy, Co. Wicklow, Ireland.
DisclaimerPrivacy PolicyTerms of UseData Deletion© Acadoodle 2026