 Video Courses
Video Courses Video Courses
Video Courses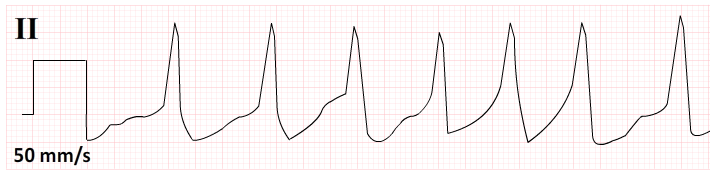
Atrial fibrillation is the most common arrhythmia encountered in clinical practice. Misdiagnosis of atrial fibrillation carries significant implications for patients. The cardinal features of atrial fibrillation are an absence of coordinated depolarisation of the atria (absence of P waves on the ECG/EKG) and unpredictable depolarisation of the ventricles (no pattern to R wave occurrence on the ECG/EKG). Fibrillation of the atria may result in a chaotic disturbance of the isoelectric line, however, this finding on an ECG can be misleading as muscular activity or agitation can cause a similar appearance. Equally, it can often be difficult to tell if P waves are present or not on an ECG. Atrial fibrillation is frequently misdiagnosed. To avoid over and under diagnosis of this arrhythmia check out the ECG section on www.acadoodle.com and follow the tips below. When faced with an ECG which raises the possibility of atrial fibrillation...
1. Not all irregular rhythms are irregularly irregular.
Ask yourself is the underlying pattern of R waves truly chaotic. If there is any pattern in the occurrence of the R waves, regular or regularly irregular, then fibrillating atria are not driving ventricular depolarisation. It can be more difficult than you might think to be sure of this. So..
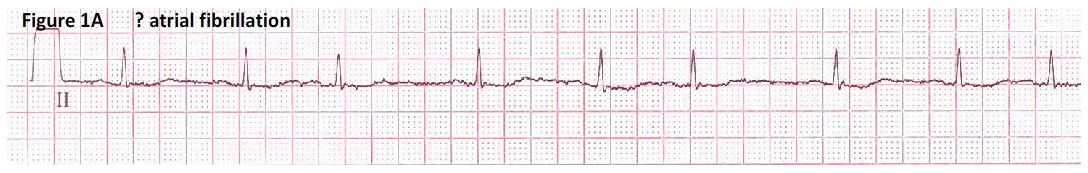
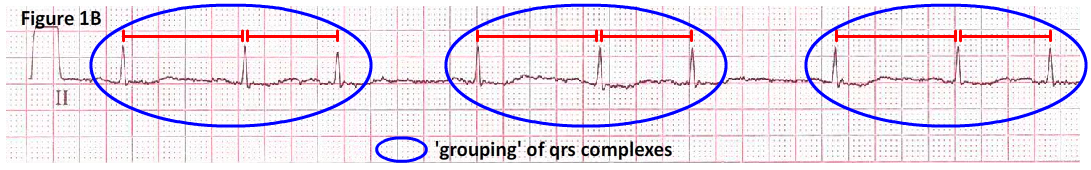
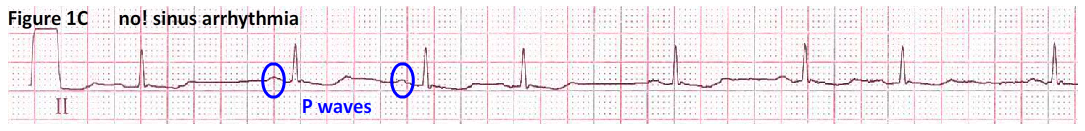
2. Look for QRS grouping.
This is a good way of looking for an underlying pattern in R wave occurrence in the presence of an irregular rhythm on the ECG/EKG. This is particularly useful if you are uncertain as to the presence or absence of P waves. Look at the rhythm strip in figure 1A, the computer interpretation and a Junior doctor have diagnosed atrial fibrillation on the basis of the irregular occurrence of R waves and failure to detect P waves. However, on closer examination of the ECG/EKG (figure 1B), a more senior doctor notices quite clear grouping of the R waves. This regularly irregular rhythm cannot be atrial fibrillation. Indeed, a repeat ECG (figure 1C) confirms the presence of P waves. This is, in fact, a marked sinus arrhythmia, an ECG finding frequently mistaken for atrial fibrillation. The patient was agitated at the time of the original ECG resulting in an arte factual disturbance of the isoelectric line making the P waves difficult to discern. This illustrates another key point in ECG interpretation. If an ECG yields an unexpected or puzzling finding, never be afraid to repeat it. This is not a sign of weakness.
3. Look carefully for evidence of coordinated atrial depolarisation.
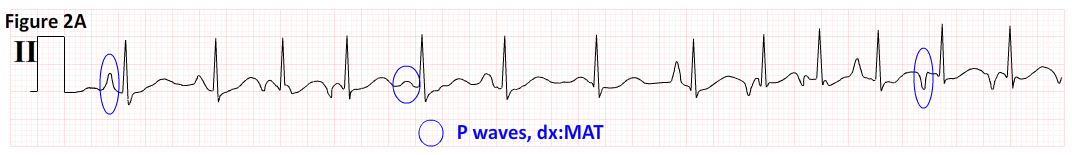
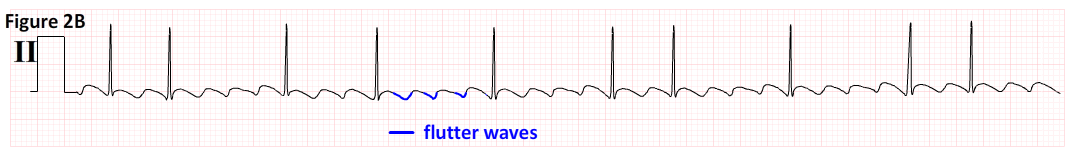
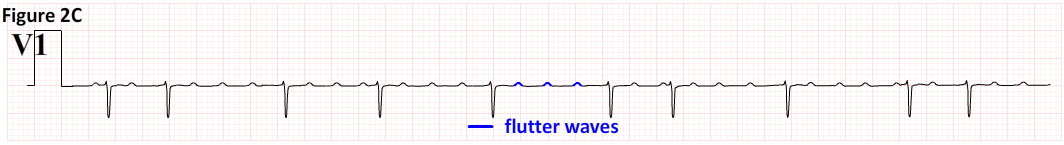
When you are happy that the occurrence of R waves is truly chaotic you must remember that atrial fibrillation is not the only cause of an irregularly irregular ventricular rhythm. Even in the presence of an irregularly irregular rhythm look carefully for evidence of coordinated atrial depolarisation. If there is any evidence of coordinated atrial depolarisation then the patient is not in atrial fibrillation (at least not sustained atrial fibrillation). Lead II is usually the best lead in which to see P waves, but this is not always the case, so look for P waves in all 12 leads. In many individuals they are best seen in lead V1. Also, remember P wave morphology may vary in certain pathologies which mimic atrial fibrillation. The relatively common arrhythmia multifocal atrial tachycardia (MAT) (figure 2A) is characterised by an irregularly irregular rhythm and P waves of multiple different timings and morphologies. MAT is frequently mistaken for, but is unrelated to, atrial fibrillation. Finally, remember atrial flutter with variable conduction will have an irregularly irregular ventricular rhythm. In this situation, provided they are looked for, runs of flutter waves in the inferior leads (figure 2B), indicating abnormal but coordinated atrial depolarisation, are usually obvious in areas where R waves are widely separated. Again, in some cases, flutter waves are best seen in lead V1 (figure 2C).
4. Consider altering the ECG/EKG ‘paper speed’.
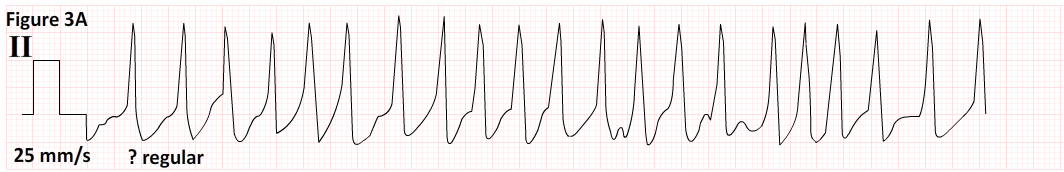
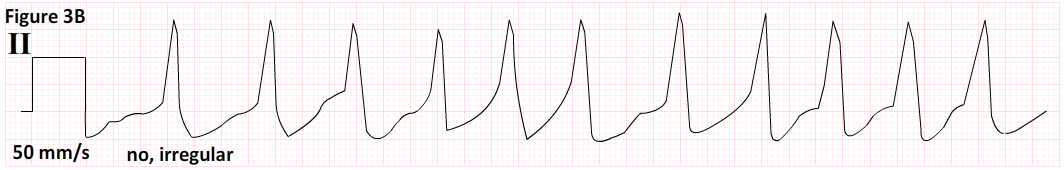
At high ventricular rates irregular rhythms may appear regular. Atrial fibrillation can be missed with serious consequences for the patient. For example, with the high ventricular rate present in figure 3A it is difficult to tell if the rhythm is irregular. However, if we double the ECG/EKG paper speed (figure 3B) the irregularity of the rhythm becomes obvious as this manoeuver doubles the distance between consecutive R waves. With an irregularly irregular ventricular rhythm, this patient may have atrial fibrillation.
5. Don’t trust the computer!
And finally, 'don’t trust the computer’. Approximately 20% of cases labelled atrial fibrillation by the computer are incorrectly interpreted and up to half of these cases are not corrected by the doctor reading the ECG! The computer would misinterpret all of the ECGs discussed in this article.
DisclaimerPrivacy PolicyTerms of UseData Deletion© Acadoodle 2025